Honours / Discipline Specific Elective (DSE)


REPRODUCTIVE BIOLOGY
►Unit 1: Reproductive Endocrinology
Mechanism of action of steroid and glycoprotein hormones. Hypothalamo – Hypophyseal –gonadal axis, regulation of gonadotrophin secretion in human (male and female); Reproductive system: Development and differentiation of gonads, genital ducts and external genitalia
Q. What is the fate of Wolffian duct?
(i)In mammals, the pronephric tubules and the anterior portion of the pronephric duct degenerate, but the more caudal portions of the pronephric duct persist and serve as the central component of the excretory system throughout its development (Toivonen 1945; Saxén 1987). This remaining duct is often referred to as the nephric or Wolffian duct.
(ii)These efferent tubules are the remnants of the mesonephric kidney, and they link the testis to the Wolffian duct, which used to be the collecting tube of the mesonephric kidney.
(iii)In males, the Wolffian duct differentiates to become the epididymis (adjacent to the testis) and the vas deferens, the tube through which the sperm pass into the urethra and out of the body.
(Meanwhile, during fetal development, the interstitial mesenchyme cells of the testes differentiate into Leydig cells, which make testosterone.)
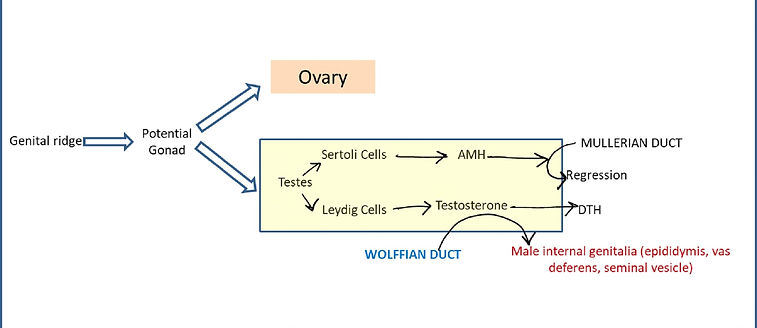
Figure: The general scheme of mammalian sex determination
(iv)The formation of the male phenotype involves the secretion of two testicular hormones. The first of these hormones is AMH, the hormone made by the Sertoli cells that causes the degeneration of the Müllerian duct. The second is the steroid testosterone, which is secreted from the fetal Leydig cells. This hormone causes the Wolffian duct to differentiate into the epididymis, vas deferens, and seminal vesicles, and it causes the urogenital swellings to develop into the scrotum and penis.
►Unit 2: Functional anatomy of male reproduction
Histoarchitechture of testis in human; Spermatogenesis and its hormonal regulation; Androgen synthesis and metabolism; Accessory glands functions
Q.What is capacitation?
Sperm capacitation refers to the physiological changes spermatozoa must undergo in order to have the ability to penetrate and fertilize an egg. This term was first coined in 1952 by Colin Russell Austin based on independent studies conducted by Austin and Min Chueh Chang and published in 1951. Capacitation does not occur until the sperm has been inside the female reproductive tract for a certain period of time. The molecular changes that account for capacitation are given as schematic presentation as follows:

►Unit 3: Functional anatomy of female reproduction
Histoarchitechture of ovary in human; Oogenesis and its hormonal regulation; Steroidogenesis and secretion of ovarian hormones; Reproductive cycles (human) and their regulation, Fertilization; Hormonal control of implantation; Hormonal regulation of gestation, pregnancy diagnosis, fetomaternal relationship; Mechanism of parturition and its hormonal regulation; Lactation and its regulation
Q. Why is progesterone needed for normal progression in pregnancy?
(i)Progesterone is responsible for the progestational changes in the endometrium and the cyclical changes in the cervix and vagina.
(ii)Progesterone causes decidual cells to develop in the uterine endometrium, and these cells then play an important role in the nutrition of the early embryo.
(iii)Progesterone has a special effect on decreasing the contractility of the pregnant uterus, thus preventing uterine contractions from causing spontaneous abortion.
(iv)Progesterone contributes to the development of the conceptus even before implantation because it specifically increases the secretions of the fallopian tubes and uterus to provide appropriate nutritive matter for the developing morula and blastocyst. There is reason to believe, too, that progesterone even atfects cell cleavage in the early-developing embryo.

►Unit 4: Reproductive Health
Infertility in male and female: causes, diagnosis and management, Assisted Reproductive Technology: Sex selection, sperm banks, frozen embryos, in vitro fertilization IVF & IUI Modern contraceptive technologies
Q. Who Can Benefit from IUI?
(a type of artificial insemination — is a procedure for treating infertility. Sperm that have been washed and concentrated are placed directly in your uterus around the time your ovary releases one or more eggs to be fertilized. The hoped-for outcome of intrauterine insemination is for the sperm to swim into the fallopian tube and fertilize a waiting egg, resulting in a normal pregnancy. Depending on the reasons for infertility, IUI can be coordinated with your normal cycle or with fertility medications)
(i)A woman has ovulation problems and has not been able to conceive using ovulation-inducing fertility medication. Fertility medication is used to increase the number of eggs a woman normally ovulates
(ii)There are minor abnormalities in the sperm analysis (such as concentration, motility, and morphology or shapes of the sperm), male partner has difficulty ejaculating
(iii)IUI is often considered as the first line of treatment for unexplained infertility, mild endometriosis, or mild male factor infertility. Donor’s sperm is being used to get pregnant
(iv)IUI can help couples where the male partner has a low sperm count or poor motility (the ability of the sperm to move), as long as there are sufficient levels of healthy, motile sperm to make the treatment worthwhile
(v)As sperm is placed directly inside the female's uterus, IUI can also help couples who are unable to have intercourse because of disability, injury, or difficulties such as premature ejaculation.
(vi)Also recommended for women with Mild Endometriosis etc.



